A 180 On Fats For Healthy Weight and Heart After decades of bad data on cholesterol and good fats, Americans are waking up to a profound new reality about their health benefits.
For over fifty years, fats have been targeted by mainstream outlets as the enemy as a prime contributor to heart disease. There has been particular emphasis on reducing cholesterol by eliminating saturated fats. In response, butter was replaced with margarine, skim or low-fat milk was recommended over whole milk, canola oil was glorified, and eggs were practically viewed as evil. Many Americans complied with these recommendations…so why, all these decades later, is cardiovascular disease still the number one cause of death in America (aside from Covid)?
Several scientists took on this question, and in January 2021, their research was published in The American Journal of Clinical Nutrition. Their work delved deeper into uncovering the cause of heart disease, pushing beyond the standard focus of what causes cardiovascular disease and asking the question “why”: considering the fact that saturated fat is naturally occurring in many foods (including breast milk) that are important to maintaining good health, why does saturated fat raise blood cholesterol, and why should cholesterol be regarded as dangerous?
With all the years of constant, convincing hype regarding the dangers of saturated fats in the diet—set within an ever-present controversy over what constitutes a healthy diet—you may well be thinking the answer is obvious—saturated fats raise cholesterol, and cholesterol leads to cardiovascular disease, right? Not so fast. The research results suggest the answers are not so cut-and-dried.
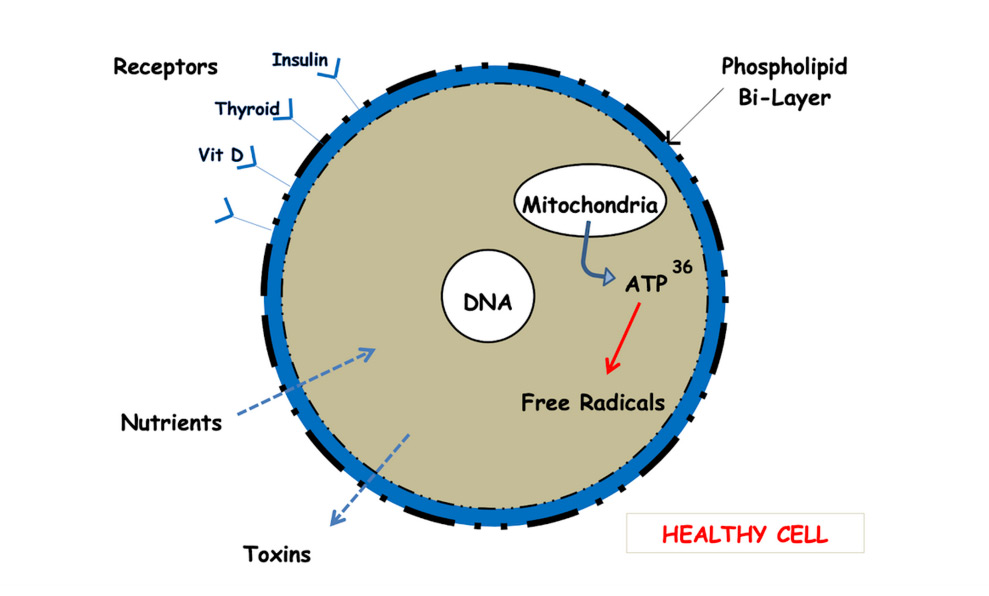
Researchers analyzed this “diet-heart hypothesis” and found an alternative explanation to the concept that saturated fats lead to high cholesterol, which in turn leads to heart disease. Their model is about what know as the “phospholipid bi-layer” [See Fig.1]. Cells, to thrive, must incorporate the necessary amounts of cholesterol molecules needed in order to prevent their outer membranes from becoming overly fluid or overly stiff. These cells change their cholesterol requirements based on a theory of homeostasis. That is, the needs of the cell will vary according to the amount of saturated or polyunsaturated fats in a person’s diet. Thus, when a diet consists of more saturated fats, cells need to absorb less cholesterol in their membranes because their surrounding environment already contains it.
Conversely, when there are mainly polyunsaturated fats (PUFAs) in a diet and the cells’ environment is more cholesterol-deprived, their membranes need to incorporate more cholesterol from their surroundings. This results in a lower blood cholesterol count in a standard fasting blood test. This provides a logical explanation as to why blood cholesterol levels can change, sometimes dramatically, particularly when there is a sharp change in fat intake.
The researchers concluded that this may be an indication as to why levels of LDL cholesterol may change even without pathology. IncreasingLDL cholesterol could be a normal cell response and is, in fact, a secondary result of insulin resistance, imbalances in the gut microbiome, endotoxemia and chronic inflammation.
Grow Your Knowledge of Functional Medicine
Sign up and receive instant access to The Root Cause Solution and begin your journey back to better health!
Sign upHealth Benefits of Good Fats
Outdated recommendations that people should eliminate fats, particularly saturated fats, from their diets caused a dangerous dietary move to include more added sugars, PUFAs, carbs, and processed foods. This led to a worldwide epidemic of overweight and obesity as well as a multitude of illnesses. For years, no differentiation was made between healthy fats and bad fats—all fats were considered equally bad and were thought to lead to high cholesterol and heart disease. Processed industrial vegetable oils such as canola, sunflower, safflower, and soybean became the recommended choices for cooking, dressings, etc.—these oils are high in omega-6 fats, which increase inflammation, the true underlying cause of serious health conditions including diabetes, cardiovascular disease, cancer, autoimmune diseases, arthritis and more. High levels of omega-6s also counteract the health benefits derived from omega-3s.
Healthy fats such as grass-fed butter and yes, even beef tallow, as well as coconut and avocado oils not only offer a wide range of health benefits, they also stand up well to cooking with high heat levels because they are not prone to oxidative damage the way other oils are. The proven benefits derived from healthy fats are actually directly opposed to the arguments against saturated fats. These benefits, among others, include:
- lowering bad cholesterol while increasing the good cholesterol
- lowering blood pressure
- lowering triglycerides
- lessening the risk of stroke and heart attack
- protection against arrhythmia
- aid in preventing and regulating mood disorders
- contribute to good mental health
- contribute to skin, hair, and eye health
- blood sugar regulation
- help with vitamin absorption
Healthy fats also allow you to feel full so you’re not craving sugars and carbs after a meal. Keep in mind that when it comes to animal fats like beef, butter, beef tallow, and other dairy, there is a big difference between products derived from grain-fed animals and grass-fed animals. Some of the benefits of nutrient-rich grass-fed animal products include:
- five times more omega-3s
- twice as much conjugated linoleic acid (CLA)
- higher carotenoid levels (precursors to vitamin A including beta carotene)
- higher levels of antioxidants including vitamin E
In addition, products derived from grain-fed animals have lower levels of natural trans fats (keep reading to understand why natural trans fats are important to good health); a diet of grains is unnatural for animals and therefore creates unhealthy changes not only for the animals but for consumers as well. Grass-fed animals are healthier in general and are typically antibiotic- and hormone-free.
Not All Trans Fats Are Equal
Trans fats as a whole are typically lumped into a single category of “unhealthy”, but there are two kinds of trans fats: natural and artificial. Moderate amounts of trans fats—CLAs—occur naturally in grass-fed animals, but less so in grain-fed animals. These natural trans fats have been shown to lower the risk of cancer and are associated with the management and prevention of diabetes through the improvement of insulin resistance and glucose tolerance as well as lowering the risk of heart disease.
On the other hand, artificial trans fats, which are found in products such as margarine, microwave popcorn, frozen pizzas, fried foods, nondairy creamers, prepared bakery goods and more, have altered chemical structures and can cause significant harm to the human body. The effects of artificial trans fats include increased inflammation and increased risk of serious health conditions including diabetes, heart disease, and others. These altered chemical structures also increase bad cholesterol while lowering good cholesterol; they also damage the lining of blood vessels.
Choosing to include healthy fats provides a wide range of foods to choose from, many of which are found in the Mediterranean diet. These choices allow for healthy trade-outs to increase nutrient density; for example, instead of coating salmon in breadcrumbs, make nut-crusted herbed salmon instead. Thinking through these substitutions, any good home cook is likely to discover some new healthier favorites!
Dr. Doug Pucci is a functional medicine practitioner who was honored in 2020 to receive both The Best Of 2020 Awards for Functional Medicine in Oradell, NJ, and entry into Trademark Publications’ Who’s Who Directory, Honors Edition, for his pioneering work. He provides comprehensive testing for health biomarkers, advanced discovery into brain/body well-being and personalized nutrition for a diversity of people and symptoms.
For more information, call 201-261-5430 or visit GetWell-Now.com